
 Above: Helga doing aquafit exercises in the neighbourhood pool
Above: Helga doing aquafit exercises in the neighbourhood pool
Written By: Heidi Singer
Photos By: John Packman
Helga Humphreys, 78, was up early one morning last summer. It was 4 a.m. and the energetic senior was puttering around her Deer Park bedroom, preparing for her daily two-kilometre walk to a downtown swimming class. That changed when she slipped and landed on her back in terrible pain.
Terrified that she had broken her spine and would end up paralyzed, Helga managed to drag herself to the kitchen phone to call 911.
It was an unfortunate moment for an independent woman who had enjoyed good health all her life. But Helga got lucky in one way — the ambulance took her to Mount Sinai Hospital’s Schwartz/Reisman Emergency Centre. In a matter of hours, she was diagnosed with a fractured spine, treated by a geriatric emergency medicine nurse and settled into a comfortable room at Bridgepoint Active Healthcare.
“It was such a relief, arriving at Bridgepoint,” recalls Helga, now back in her apartment and steadily recovering her mobility. “I went from a little gurney in a hallway with lights flashing and things beeping and a lot of traumas going on, to a room with a pleasant view and friendly staff. I was so amazed; I couldn’t believe it.”
All too often, stories about the world of emergency medicine tell of events that go badly wrong. This is a story of everything that went right —when bureaucracy didn’t get in the way, when staff were plugged into a network of resources and the right care was delivered at the right time. It’s a glimpse into the kind of care that Sinai Health System is actively working toward, where emergency management is fully, deeply connected to the rest of the medical system, where diagnosis, treatment and transition are handled seamlessly.
In less than a decade, the number of patients coming through one of the city’s smallest emergency departments (EDs) has doubled. Staff responded with an array of evidence-based changes that cut wait times in half, to the shortest in the city. Still, walk into the ED on any given day and you’ll see stretchers full of patients lining the hallways.
To cope with this growth, Mount Sinai will soon see even bigger changes. The hospital is embarking on an ambitious expansion and renovation that will more than double its space, to 28,000 square feet, add new technology with the capacity to treat 80,000 patients a year and reorganize care based on the best evidence. The redesign will be senior-friendly, with more washrooms and handrails, and more clocks and natural light to keep people oriented.
 The revitalized ED will have more isolation rooms for people with suspected cases of infectious disease like tuberculosis and even the flu. Hand sanitizers and hand-washing stations will be placed to encourage maximum use. Seven nursing stations (there are currently three) will be located to maximize the number of patients in the direct eyesight of staff. There will be a separate entrance for patients arriving by ambulance or police. And the department will have its own next-generation CT scanner and X-ray.
The revitalized ED will have more isolation rooms for people with suspected cases of infectious disease like tuberculosis and even the flu. Hand sanitizers and hand-washing stations will be placed to encourage maximum use. Seven nursing stations (there are currently three) will be located to maximize the number of patients in the direct eyesight of staff. There will be a separate entrance for patients arriving by ambulance or police. And the department will have its own next-generation CT scanner and X-ray.
The goal is for success stories like Helga’s to become commonplace. But timely care isn’t just a matter of convenience, says Dr. Howard Ovens, Chief of Emergency Medicine. Extensive research shows that longer wait times mean higher risks for hospital-acquired infection and accidents. Overstretched EDs are associated with more mistakes and worse health outcomes.
“The philosophy is the right care at the right place at the right time,” says Dr. Ovens, who is also the Ontario Provincial Expert Lead in Emergency Medicine. “Helga didn’t need all the sophisticated diagnostic facilities of an acute care hospital, but she did need intensive rehabilitation, and she would get more of that at Bridgepoint, in a more homelike setting.” Timely care meant that she started physiotherapy on the day of her injury — not days or even weeks later.
“The speed with which staff were able to transfer Helga to Bridgepoint is highly unusual for any hospital, probably anywhere in the world,” Dr. Ovens says. Under normal procedures, “she would have been admitted to the hospital during the paperwork and application process, so there would be a stay of at least a few days that would add almost no value to her care.”
Helga’s experience illustrates the possibilities of “connected care,” an idea that hospital staff and health leaders are eagerly putting into practice. Last year, Mount Sinai Hospital and its research arm, the Lunenfeld-Tanenbaum Research Institute, joined with Bridgepoint and Circle of Care to form Sinai Health System. That connection allowed ED staff to transfer Helga straight from a hallway stretcher to a rehabilitation unit.
“It’s great to have a partnership with an acute care facility,” says Heather Kwok, Clinical Practice Lead for Physiotherapy at Bridgepoint. “At a hospital, patients aren’t as active as they could be. This can delay recovery. The earlier you get rehab, the shorter your recovery time and the faster you can return to the community.” This, in turn, frees up precious space at Bridgepoint for the next patient.
 Above: Heather Kwok, Clinical Practice Lead for Physiotherapy, in the BMO Financial Group Therapy Gym at Bridgepoint
Above: Heather Kwok, Clinical Practice Lead for Physiotherapy, in the BMO Financial Group Therapy Gym at Bridgepoint
Social worker Rebecca Detje, who was instrumental in finding Helga a place at Bridgepoint, helped her understand what was happening every step of the way. “Many people are intimidated, staying in the hospital needing an uncertain element like rehab,” Ms. Detje says. “So being able to let them know right away where they’ll go and when they’ll be on their way is usually reassuring. I think Helga’s experience is a really positive example of the possibilities for collaborative work inside the ED, as well as between the ED and rehab at Bridgepoint.”
“We can’t control how long it takes to get imaging and test results. One of the few things we can control in the ED is who needs what care and how do we best treat them?”
- Dr. Bjug Borgundvaaag , Emergency Physician and Researcher
Understanding how her care would unfold brought Helga a peace of mind that enabled her to make some decisions. She recalls lying on the hallway gurney, groggy from painkillers and worrying that her daughter didn’t know what had happened. But she was equally concerned about the panic that a phone call from an emergency room would cause. Knowing that she would be comfortably settled at Bridgepoint by the afternoon helped her decide to postpone calling until then.
Connecting patients to the right care at the right time has ripple effects that extend beyond the patients’ own experience. With Ontario’s growing and aging population, the strain on hospital resources is like a coming tsunami. In the crowded ED that summer afternoon, one fewer patient took up a valuable stretcher; one fewer patient was admitted to a ward upstairs to wait for a spot in a rehab facility. What if Helga’s experience, admittedly a small victory for the health of Ontario’s health system, could be multiplied by hundreds every day, in every emergency department in Toronto?
Nobody can control the ebb and flow of patients who need emergency care. That’s where Dr. Bjug Borgundvaaag comes in. Dr. Borgundvaag is an emergency physician and researcher specializing in finding the sweet spot where the best care and the most efficient delivery meet. Recently, he helped develop a way for ED staff to more accurately treat patients in alcohol withdrawal, cutting an average of three hours off their care. And Dr. Borgundvaag has helped determine when patients with infections, pregnancy complications or congestive heart failure need immediate hospitalization and when they can be sent home.
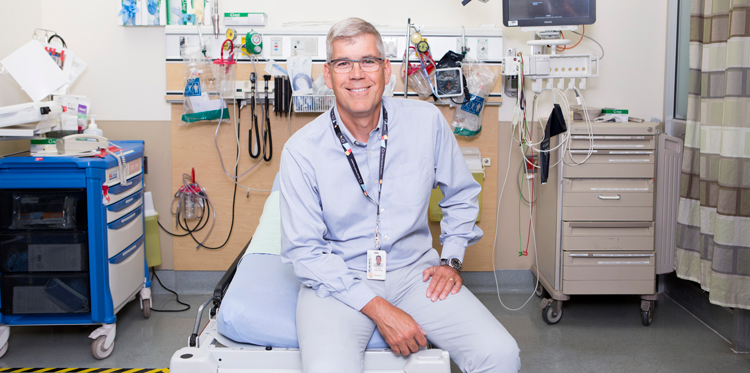 Above: Dr. Bjug Borgundvaag, Director, Schwartz/Reisman Emergency Medicine Institute
Above: Dr. Bjug Borgundvaag, Director, Schwartz/Reisman Emergency Medicine Institute
“Our work is geared toward common problems that we see lots of — areas where there’s a great opportunity to improve care,” says Dr. Borgundvaag. “We can’t control how long it takes to get imaging and test results. Blood tests take a certain amount of time. And we can’t control how long it takes for patients to move out of the ED and up to a bed. One of the few things we can control in the ED is who needs what care and how do we best treat them?”
Dr. Borgundvaag is the inaugural director of Canada’s first emergency academic institute, the Schwartz/Reisman Emergency Medicine Institute. His research has directly contributed to the lowering of waiting times in Mount Sinai’s ED in recent years. Now, as part of the new Sinai Health System, he will have access to more data to inform future research.
“Information in the ED is one of the hardest things to get your hands on, especially when you need it for a patient you’re transferring,” he says. “That’s why I have high hopes that our partnership with Bridgepoint and Circle of Care will help us expedite people to the right level of care.”
Dr. Borgundvaag’s work has been greatly helped by the vision of supporters like Gerald Schwartz, CEO of Onex Corporation and former Vice-Chair of Mount Sinai Hospital, and his wife, Heather Reisman, CEO of Indigo Books and a member of Sinai Health System’s Board of Directors. Understanding that care is only as good as the evidence that underpins it, the couple established the research and knowledge translation centre, which boasts a director and three researcher-clinicians. In total, they have given $15 million toward both the Schwartz/Reisman Emergency Medicine Institute and the Schwartz/Reisman Emergency Centre expansion — allowing hospital leaders to build a state-of-the-art facility that could become a model for other Canadian emergency rooms. Their management expertise has been particularly helpful to hospital leaders in rethinking the layout and patient flow of the new ED.
 Another pair of long-term supporters, Howard Sokolowski, O.Ont., Co-Chair of Sinai Health Foundation’s Board of Directors, and his wife, the Honourable Linda Frum, a Sinai Health System Board Member, have generously donated $7 million toward the project, including $1 million for research. Patients will feel the impact of their generosity in many ways, but most visibly, the current, tightly packed ED waiting room will be replaced by a new, family-friendly space, named the Sokolowski/Frum Reception, Triage and Waiting Area.
Another pair of long-term supporters, Howard Sokolowski, O.Ont., Co-Chair of Sinai Health Foundation’s Board of Directors, and his wife, the Honourable Linda Frum, a Sinai Health System Board Member, have generously donated $7 million toward the project, including $1 million for research. Patients will feel the impact of their generosity in many ways, but most visibly, the current, tightly packed ED waiting room will be replaced by a new, family-friendly space, named the Sokolowski/Frum Reception, Triage and Waiting Area.
“Their support, interest and also their expectations — their polite way of challenging us — is a big part of our success,” says Dr. Ovens. “I’m personally so grateful for the variety of ways they elevate our performance.”
These gifts are part of the Sinai Health System’s “Campaign to Renew Sinai”, which is helping to transform the facilities and delivery of care across the entire system and grow many of its internationally-recognized clinical and research programs.
The ambition is huge, but the payoff is already being felt. For Helga, the right care at the right time brought her home faster — and back to her morning stroll, albeit shorter and with a walker for now.
“I do everything myself,” she says, sitting at the kitchen table of her immaculate apartment with its beautiful city views. She vividly remembers how the fear and pain of that morning gave way to comfort and reassurance, and by nightfall, she can even recall thinking, ‘My God, it’s my lucky day.”